
Incidence

It is estimated that 1 out of 8 women will develop breast cancer over their lifetime. In Switzerland, breast cancer is the most frequent form of cancer and the main cause of cancer deaths in women aged between 50 and 70 years. Each year about 7’000 women are diagnosed and more than 1’500 die from the disease.
Symptoms
The first symptom of breast cancer most people notice is a new lump or some thickening in their breast or armpit. Other symptoms include:
- a change in size, shape or feel of your breast
- skin changes in the breast such as puckering, dimpling, a rash or redness of the skin
- fluid leaking from the nipple in a woman who isn’t pregnant or breastfeeding
- changes in the position of the nipple
Causes
The exact causes of breast cancer are not fully understood. However, there are certain factors known to increase the risk of breast cancer. These include:
- age – the risk increases as you get older
- a family history of breast cancer*
- a previous diagnosis of breast cancer
- a previous non-cancerous (benign) breast lump
- being tall, overweight or obese
- drinking alcohol
*Inherited gene changes: Some gene changes (mutations) are inherited or passed to you from your parents. Certain inherited gene changes can greatly increase the risk for developing certain cancers. Genetic testing can identify some women who have inherited mutations in the BRCA1 or BRCA2 tumor suppressor genes as well as other less common genes such as PALB2, ATM, or CHEK2. These women can then take steps to reduce their risk of breast cancer by increasing awareness of their breasts and following appropriate screening recommendations to help find cancer at an earlier, more treatable stage. However, most gene mutations linked to breast cancer are acquired, this means the change takes place in breast cells during a person’s life rather than having been inherited or born with them. These acquired mutations of oncogenes and/or tumor suppressor genes may result from other factors, like radiation or cancer-causing chemicals. But some gene changes may just be random events that sometimes happen inside a cell, without having an outside cause.
Subtypes
There are many different types of breast cancer. The type is determined by the specific kind of cells in the breast that are affected. Most breast cancers are carcinomas. The most common breast cancers such as ductal carcinoma in situ (DCIS) and invasive carcinoma are adenocarcinomas since the cancers start in the gland cells in the milk ducts or the lobules (milk-producing glands). Breast cancers are also classified by certain types of proteins or genes expressed. After a biopsy is done, breast cancer cells are tested for proteins called estrogen receptors and progesterone receptors, and the HER2 gene or protein. The tumor cells are then analysed to find out what grade it is.
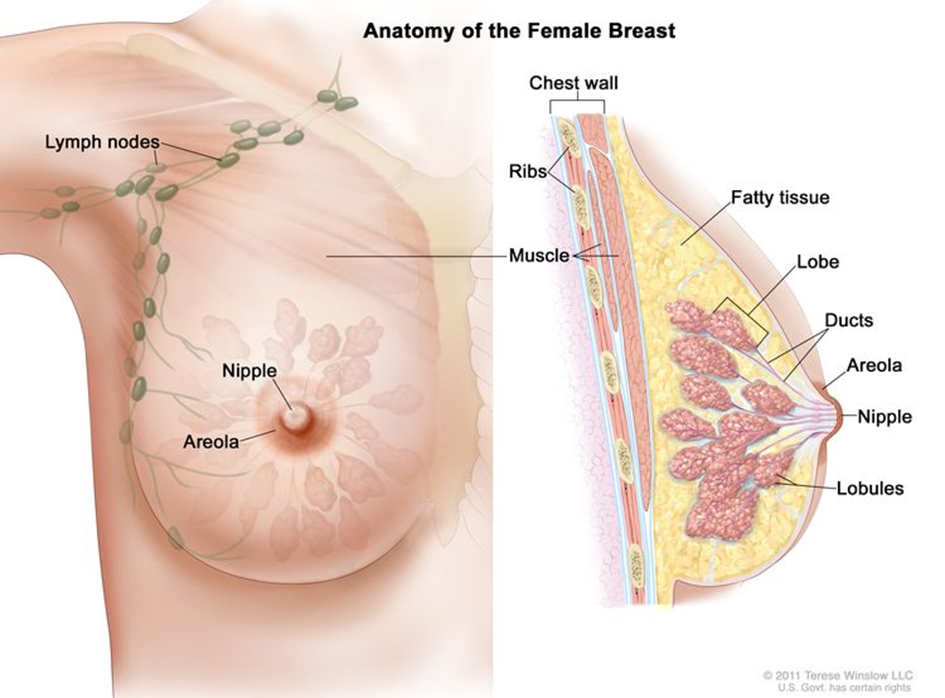
The breast is made up of lobes and ducts. Each breast has 15 to 20 sections called lobes, which have many smaller sections called lobules. Lobules end in dozens of tiny bulbs that can produce milk. The lobes, lobules, and bulbs are linked by thin tubes called ducts. Each breast also has blood vessels and lymph vessels.
Survival
Survival depends on many different factors such as type and stage of cancer, level of fitness or previous treatments. Survival for breast cancer is generally good, particularly if you are diagnosed early. Screening, early diagnosis and improved treatment options have increased the survival rates in the past years.
Treatment
If cancer is detected at an early stage it can be treated before it spreads to other parts of the body. Surgery is usually the first type of treatment, followed by chemotherapy or radiotherapy or, in some cases, hormone or targeted treatments. The type of surgery and the treatment afterwards will depend on the type of breast cancer. Your doctor should discuss the best treatment plan with you.
> For more information visit:
Screening
Cancer screening involves testing apparently healthy people for signs that could show that a cancer is developing. It is important to remember that screening will not prevent you from getting breast cancer but aims to find early breast cancers. Overall, the breast screening programme finds cancer in around 9 out of every 1,000 women having screening.
Mammography, where X-ray images of the breast are taken, is the most commonly available way of finding a change in your breast tissue (lesion) at an early stage. However, you should be aware that a mammogram might fail to detect some breast cancers and it has also some important limitations such as low screening sensitivity and specificity, risk of significant overdiagnosis and risk for cumulative radiation inducing DNA damage in particular for patients with DNA repair defects (e.g. BRCA1/2 mutations). Additionally, it is not recommended before the age of 50, despite the fact that 20-25% of breast cancers appear before this age.
Other screening tests include the following:
- Laboratory tests: Medical procedures that test samples of tissue, blood, urine, or other substances in the body.
- Genetic tests: A laboratory test in which cells or tissue are analyzed to look for changes in genes or chromosomes.
For relapsing (metastatic) breast cancers there are no validated tests. Thus, there is a need for better tests for breast cancer screening and monitoring.
> For more information about screening visit:
https://www.swisscancerscreening.ch
https://www.cancer.gov/types/breast/patient/breast-screening-pdq
Prevention
As the causes of breast cancer are not fully understood, at the moment it’s not possible to know if it can be prevented. Several studies have analysed the link between breast cancer and diet. Although there are no clear conclusions, there are benefits for women who:
- mantain a healthy weight
- excercise regularly
- have a low intake of saturated fat
- do not drink alcohol

Finally, breast self-examination or self-palpation are simple gestures which, when performed regularly, allow you to know your breasts well, detect any abnomality and report it to your doctor. The self-examination constitutes an additional asset for your health but in no way replaces your regular (at least annual) visit to your gynecologist or doctor. In case of doubt or question after a self-examination, consult your general practitioner or gynecologist.
> For more information about prevention visit:
https://www.cancerdusein.org/les-cancers-du-sein/le-depistage-precoce/lauto-examen-des-seins
